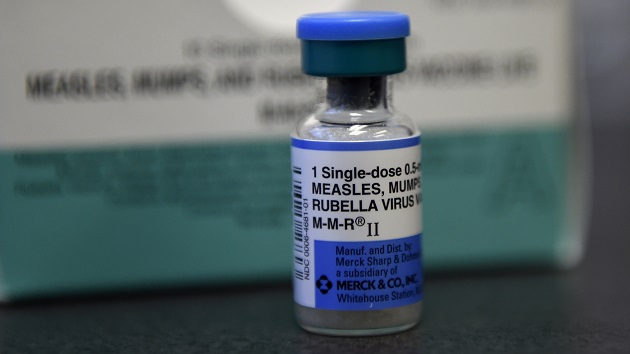
(NEW YORK) — Most counties in the United States have seen a decline in childhood measles, mumps and rubella vaccination rates over the last five years, according to a new report published Monday.
Researchers from Johns Hopkins University looked at data from 2,066 counties across 33 states between 2019 and 2024. They found that 78% of the counties, or 1,614, reported a decrease in vaccination rates over that period.
What’s more, the average vaccination rate fell from 93.92% pre-pandemic to 91.26% post-pandemic, according to the report. This represents a decline of about 3%.
Researchers also found that just four states — California, Connecticut, Maine and New York — had an increase in county-level vaccination rates.
“Measles outbreaks happen within a community, and so it’s really important to understand vaccination coverage at a higher resolution than the state level,” senior author Lauren Gardner, director of Johns Hopkins University’s Center for Systems Science and Engineering, told ABC News.
“You could have a state level average that is around 95%, which looks pretty good and makes it seem like that state is protected but, in reality, you may have a situation where you have a group of counties with coverage around 100% and another group of counties with coverage that’s 90% or below. So, you actually really have a lot at risk,” she continued.
Gardner said this report is the first to examine counties to identify trends in vaccination rates using such a comprehensive dataset, and it mirrors national trends, showing a lag in MMR vaccinations.
During the 2023 to 2024 school year, 92.7% of kindergartners received the MMR vaccine, according to data from the Centers for Disease Control and Prevention (CDC). This is lower than the 93.1% seen in the previous school year and the 95.2% seen in the 2019 to 2020 school year, prior to the COVID-19 pandemic.
It comes as the U.S. has been facing a rise in measles cases across the country amid outbreaks in states such as Texas and New Mexico.
As of Friday, a total of 1,088 cases have been confirmed in 32 states this year, according to the CDC. This marks the first time the U.S. has surpassed 1,000 cases in five years.
Among the nationally confirmed cases, CDC says about 96% are among people who are unvaccinated or whose vaccination status is unknown.
Three measles deaths have occurred so far this year, two among children and one in an adult, all of whom were unvaccinated.
Measles was declared eliminated from the U.S. in 2000, but declining vaccination rates have led to outbreaks over the last several years.
The Johns Hopkins researchers noted that if vaccination rates continue to decline, the U.S. could be at risk of measles becoming endemic.
“I hope that [the report] sheds light on the importance of vaccination and the fact that we have a problem in this country right now with vaccination rates dropping in a lot of locations, and that this poses a risk to a lot of communities, but that it’s a recoverable problem and something that we can fix,” Gardner said.
The CDC currently recommends that people receive two vaccine doses — the first at 12 to 15 months and the second between 4 and 6 years old. One dose is 93% effective, and two doses are 97% effective against measles, the CDC says.
Previous studies have shown that even a small uptick in vaccination could prevent millions of measles cases in the U.S.
“It’s a very preventable problem,” Gardner said. “We have a very safe and very effective vaccine that is available, and so I think I would like people to take away that this is a problem right now, but it’s a problem that we can overcome.”
The report did not look at why MMR vaccination rates are declining, but Dr. Whitney Harrington, an associate professor of pediatric infectious diseases at the University of Washington, who was not involved in the study, said there are likely a couple of reasons, including less exposure to the disease.
“In the case of MMR, historically, we’ve been very close to elimination within the United States, and that makes it hard to understand the rationale for being vaccinated or getting your children vaccinated,” she told ABC News. “And then I think, in combination, as we’ve seen less exposure to these diseases, at the same time, there’s been rising concern about safety of vaccines, and more vaccine hesitancy among parents and families.”
She said that any parents who are vaccine-hesitant should speak with their health care provider about the benefits of vaccination.
“I ask families, ‘What questions do you have?” rather than ‘Do you have questions?'” she said. “I think it’s much more effective to say, ‘Are there concerns that you have, or there are questions that I can answer for you about the safety of this vaccine, or about the disease that that were preventing’ and I think being able to share with family what its he disease that we’re trying to prevent can be really helpful.”
Dr. Keerthana Pakanati is a cardiovascular disease fellow at Virginia Mason Franciscan Health and a member of the ABC News Medical Unit.
Copyright © 2025, ABC Audio. All rights reserved.
